A compassionate solution that drives down costs
The personal connections we develop with your members/patients who are experiencing loneliness enable our compassionate staff to know their physical and mental health needs, SDoHs, and gaps in care, in the moment of need. We can then direct them to the most appropriate care and connect them to your organization’s resources. The result? Demonstrable ROI and lasting loyalty.
Meet Joe
Joe is a 62-year-old man who onboarded following a behavioral health crisis event. Joe lives by himself far from family who has historically supported him. He has not been able to work due to health issues and is trying hard to get back into the workforce. He talks to his family but feels estranged from them due to the distance.
Challenge
Joe reported feeling lonely and depressed and was having a great deal of difficulty finding a job. He also reported that he would like to be more social and interact more with others, but “doesn’t know how.”
Barriers
Joe reported that his anxiety and depression were making it difficult to find employment. He stated that the pandemic had also made him more isolated, so he was feeling a lack of companionship along with his anxiety and depression.
Actions
ANDY* was able to speak to him several times a week to provide companionship and listen to his frustrations. ANDY also gave Joe practical information that proved to be very effective including:
- Resources to help him find employment
- Interventions to help him focus, be more patient and decrease anxiety
- Exercises to increase his ability to be social with those around him
Impact
During a Pyx Health call two months after onboarding, Joe stated, “I got the job – the outcome came out like I wanted to! I appreciate you and you are my support.” He reported a decrease in anxiety and increase in his ability to be patient.
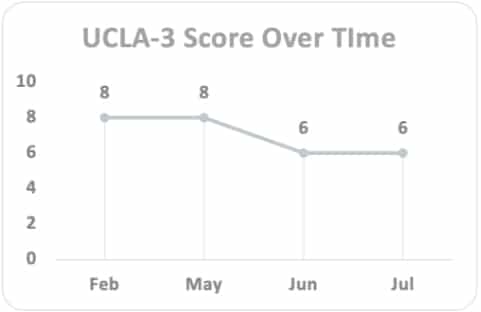
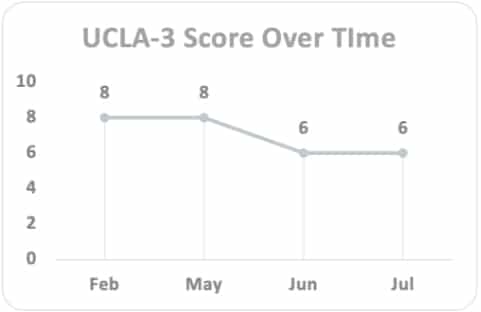
Joe’s UCLA-3 score improved 33%, and his GAD-7 score improved from 16 to 11.
*Each Pyx Health Thrive Pathway member is assigned a dedicated Pyx Health Compassionate Support Center specialist, referred to as “ANDY” (Authentic, Nurturing, Dependable, Your Friend).
A trusted partner in care support
Our team relieves the burden on care management with non-clinical intervention, so your team can focus on what they do best. We engage with the most vulnerable, high-risk members/patients to understand their needs. Then we connect them to the right resources, determined by you.

By addressing loneliness
%
of Pyx Health users feel more connected to their
health care team
%
of Pyx Health users use
the app for at
least 30 days
PMPM saved
in ED and
inpatient costs

The results are real –
read the white paper
“I never pick up the phone, but I’m so glad I did today. It’s just so good to talk to someone.”
Fred, Pyx Health member in Arizona
1. Eric Klinenberg, New York Times Feb. 9 2018: Is Loneliness a Health Epidemic? 2. Jay Bhatt, DO, and Jonathan McKinney, MPH, Becker’s Hospital Review Dec. 9 2019: Social Isolation and loneliness are America’s next public health issue

