Health Plan Member Solutions: Activate Members, Improve Outcomes
Connecting with people in ways that change patterns and unlock access to the care they’ve been going without.
Beyond Engagement: the Power of Member Activation
Pyx Health activates sustainable improvement – for health plans and their members. To help health plans engage the members who are hardest to reach, we blend personalized technology, real human connection, and home-delivered resources that identify hidden risks, close gaps in care, and address unmet social needs. Because overcoming barriers to care efficiently delivers better outcomes for members and stronger impacts for the plan’s bottom line.
%
of members highly satisfied with Pyx Health
%
decrease in
“unhealthy days”
per month
%
engagement in
Pyx Health program
100%|49.8%|56%
HRA completion rate|engagement rate for DSNP members|reported first trimester prenatal visit data
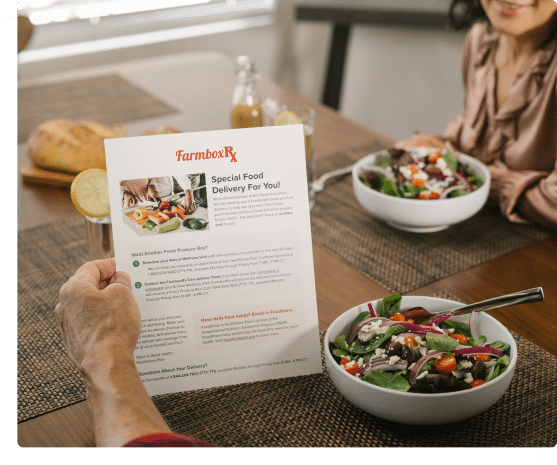
Food Opens the Door. Continuous Engagement Closes the Gap.
Every member’s health journey is different. But for many, there are real, emotional, social, and logistical barriers that stand in their way. When those needs go unmet, costs increase, quality metrics decrease, and people go without the care they need.
This is where we do our best work. We shine a light on hidden risks and barriers that typically go unseen, and support members in taking action, even when care has long felt out of reach. Our high-touch approach builds trust by meeting people where they are: whether that’s with a fresh box of food at the door, a text message that shows up at just the right time, or with a real human on the phone—someone who listens, connects, and helps inspire them to make real change.
From there, our continuous engagement activates members to become active participants in their health journey, impacting plans by improving outcomes, closing care gaps, reducing utilization, and saving money while doing right by the people they serve.
Food Opens the Door
A home-delivered box of food meets members where they are, literally. But it’s more than just a box of food, Pyx Health delivers your messages and cultivates connection with your health plan members. Building trust, inspiring self-efficacy, and promoting action while creating lasting behavioral change. Through that process, we work with plans to support:
Member health outcomes
Cost savings through preventative care
Engagement with quality initiatives
Improved member satisfaction
Long-term member retention
Reduction in high-cost claims
Overall membership growth
Accurate and timely risk score coding

Rewards and Incentives
Use a home-delivered food or wellness box as the delightful referrable moment to make meaningful connections and inspire action to help close your quality care gaps.

Benefits
Differentiate your rich benefits to improve retention and satisfaction while building a strong relationship with your members.
Continuous Engagement Closes the Gap
Engagement
At Pyx Health, our messages get attention. Our proprietary algorithms provide insights on what matters most to members, allowing us to meet them where they are, with messaging relevant to them.
Our proprietary Loneliness Index identifies members most in need of support, who are also least likely to raise their hand, while our SDoH index identifies members most likely to need help removing barriers to care, allowing our team to engage and provide actionable support where members need it most.

Activation
We can do more with each interaction. We connect with empathy and lived experience, allowing us to transform a transactional contact into multiple, meaningful interactions that meet both member and health plan goals.

Our remote care coordinators deliver personalized coordination and resource navigation, along with empathy-led coaching for behavior change and self-reliance.

Our 24/7 accessible app-based platform technology is backed by science, easy to use, and includes member tools, screenings and configureable resources
Impact
We make the most of the time we have with your members. We don’t just identify problems, we help members solve them through intensive care coordination, peer-to-peer connection, resource navigation and closed loop support.
We specialize in hard-to-reach and high-need populations – DSNP, maternal, and vulnerable children and families. In addition to ongoing support of these populations, we can also help health plans with:
Who We Serve
We work with health plans across the country to make an impact on a variety of populations, including maternal, family (CHIP), seniors, DSNP, SMI, diabetes, and more.
serving all 50 states
client NPS
covered lives
health plan partners
Loneliness, evolved
Pyx Health entered the market in 2017 with the laser-focused mission to reduce loneliness as a root cause of myriad physical and behavioral health issues for vulnerable populations. How did we do that? Simply put, we connected: We reached out. We listened. We empathized. And we acted.
Today Pyx Health is looking beyond loneliness to members’ and health plans’ evolving needs to imagine new solutions and create new programs that impact process and outcomes, while remaining mission focused. We’re using what we’ve learned about connection to redefine engagement and create trusted relationships that truly activate members. Because no one gets better alone.
Leading the way. Pyx Health is recognized as a trusted, effective leader in member engagement and care coordination.